- Latest IDSA clinical practice guideline for management of candidiasis
- Latest ACR expert panel on urologic imaging of recurrent lower urinary tract infections in women
Latest Updates

Unstable Angina and Non-ST Segment Elevation Acute Coronary Syndrome
- Beta blockers remain underused in clinical practice despite demonstrated efficacy in acute myocardial infarction (AMI). They have been shown to reduce myocardial oxygen demand and infarction size, and alleviate AMI-related pain. They also reduce the likelihood of developing mechanical and arrhythmogenic complications of AMI. They can be dosed in a wide range, and should be started at the lower end of the dosing range and titrated upward. The only relative contraindications to treatment with beta blockers are mild to moderate heart failure, obstructive airway disease (in the absence of asthma), peripheral vascular disease, diabetes mellitus and a history of cardiomyopathy.
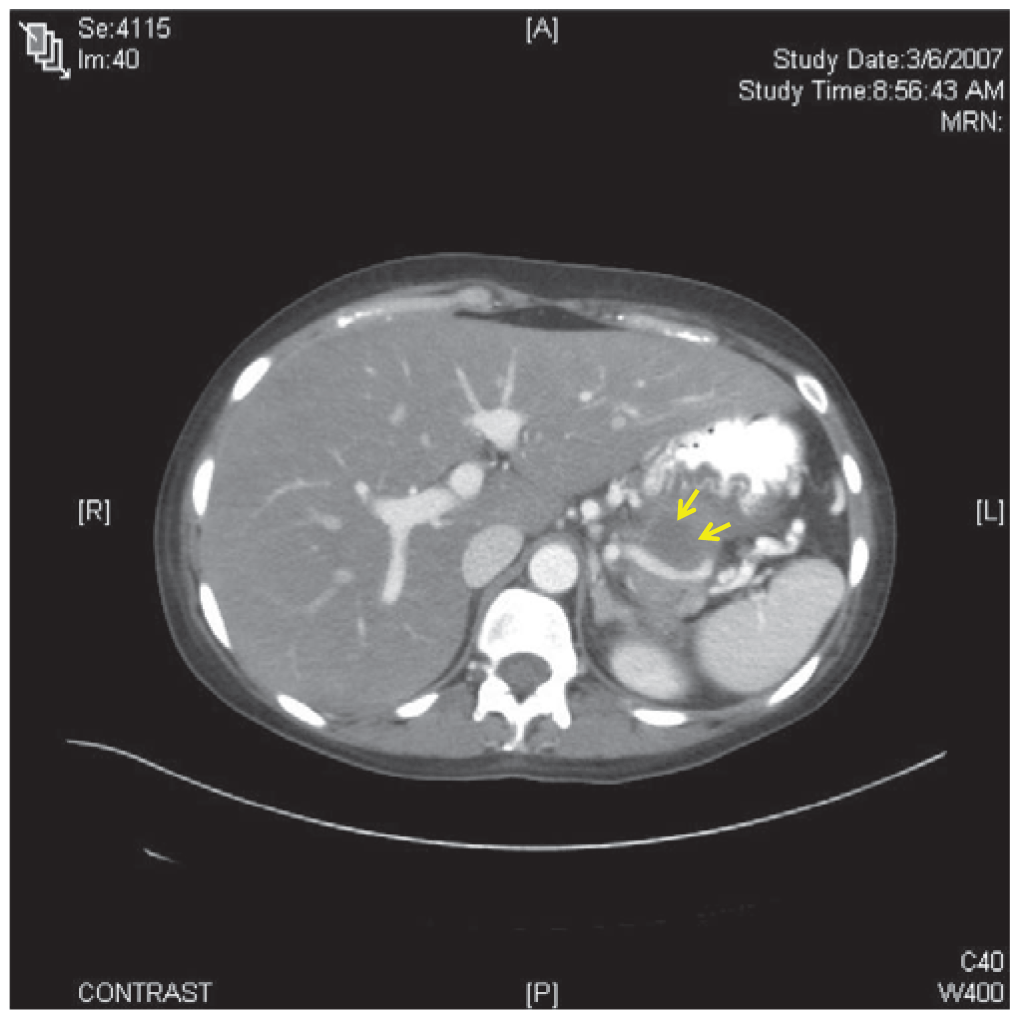
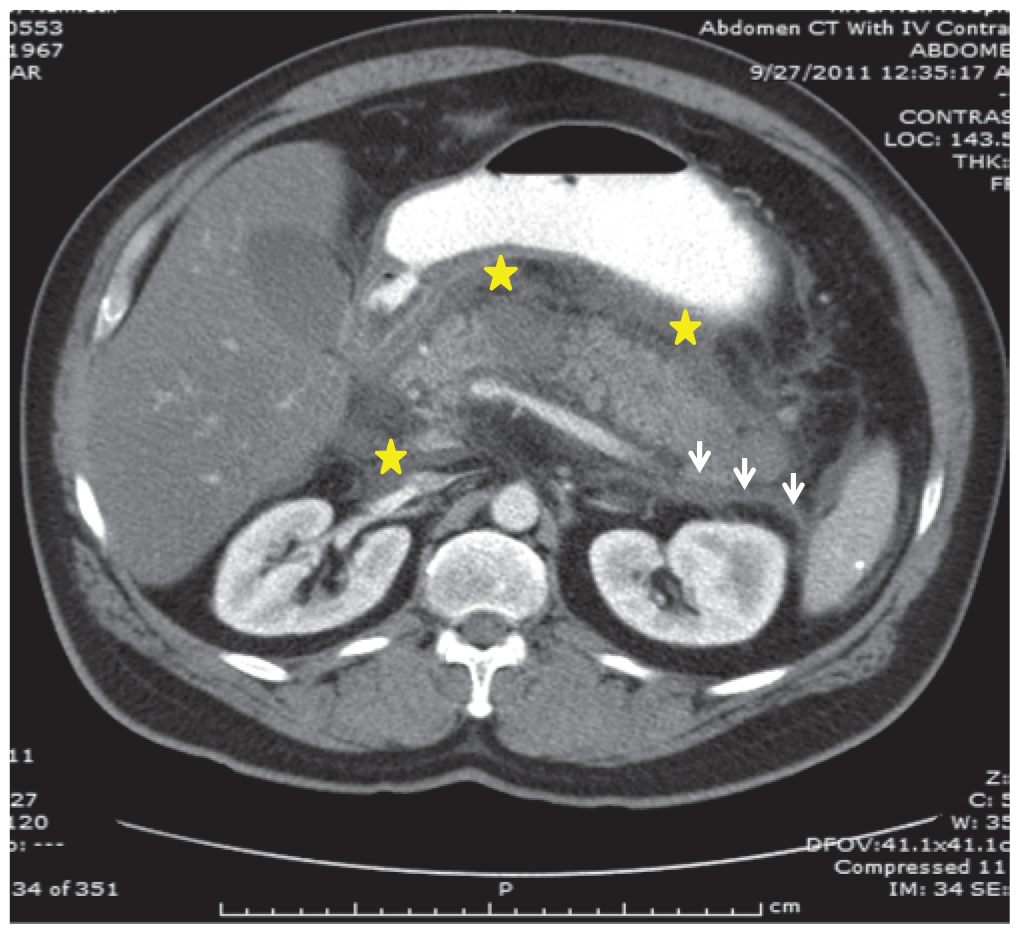
- The chief presenting complaint in acute pancreatitis is abdominal pain. The differential diagnosis for pancreatitis is broad, and includes abdominal, pulmonary, urologic and cardiovascular pathologies.
- Recent guidelines state that the diagnosis of acute pancreatitis should be established by meeting two of the following clinical, laboratory, or imaging criteria: abdominal pain and examination consistent with the disease, a serum amylase and/or lipase three times the upper limit of normal, and/or computed tomography, magnetic resonance imaging, or ultrasonography findings consistent with the disease.

Disorders of Acid-Base and Potassium Balance
- Latest evidence-based management of potassium disorders.
Shock: Pathophysiology and Management
- The importance of prompt administration of intravenous fluids and vasoactive medications (norepinephrine or dopamine as the first choice) and the limitations of protocol-based therapy, as guided by recent evidence, should be emphasized.
- There is significant controversy surrounding Early Goal-Directed Therapy (EGDT) in the management of severe sepsis and septic shock. Recently, a few, large, multicenter randomized trials, including ProCESS (Protocolized Care for Early Septic Shock), ARISE (Australasian Resuscitation in Sepsis Evaluation), and ProMISe (Protocolised Management In Sepsis) failed to provide similar conclusive supporting evidences.

- Bedside right lower quadrant ultrasonography to assess for acute appendicitis is rapid and noninvasive and does not involve ionizing radiation. Studies have validated that nonradiologist clinicians, when trained properly, can safely and accurately perform this examination, with sensitivities and specificities similar to those achieved by radiologists.
- Ultrasonographic detection of either a complex fluid collection or abscess is reported to be 99% specific for diagnosis of a perforated appendix but only 36% sensitive.
- A recent randomized controlled trial of amoxicillin-clavulanate versus appendectomy demonstrated the noninferiority of antibiotics for treatment of acute noncomplicated appendicitis but did not demonstrate an increased rate of complications in the appendectomy group. However, a Cochrane review of antibiotic therapy versus operative management did not find conclusive data to support antibiotic therapy and concluded that appendectomy remains the gold standard treatment.
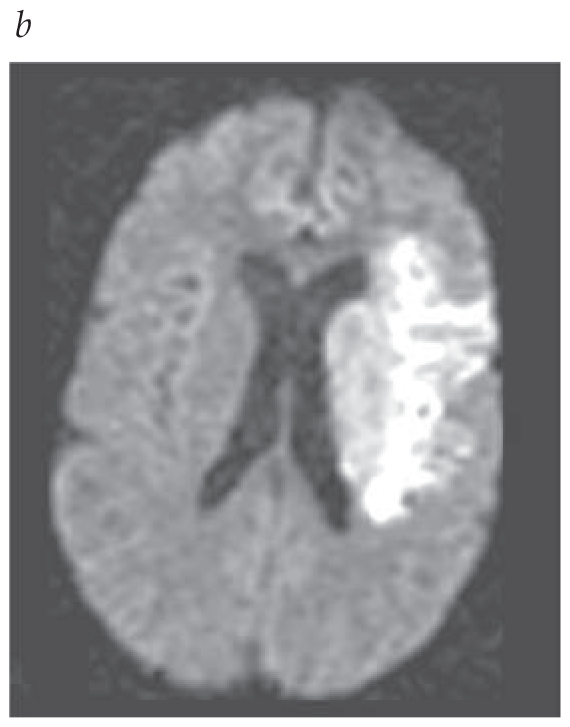
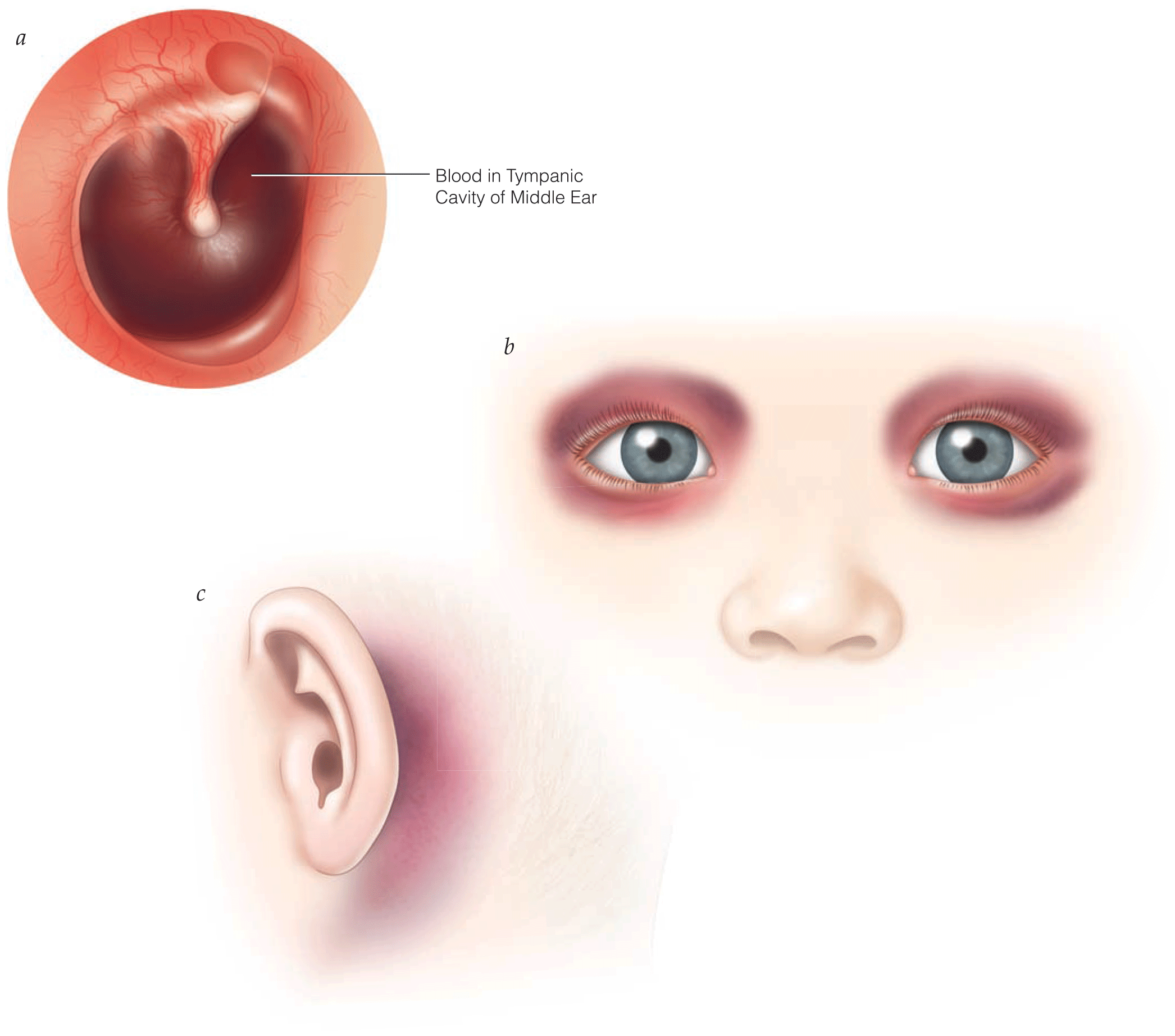
Acute Ischemic Stroke and Transient Ischemic Attack
- Endovascular treatment of acute ischemic stroke (AIS) enables access to occluded intracranial vessels for local administration of thrombolytics, mechanical embolectomy, and/or angioplasty. There are currently four mechanical devices cleared by the Food and Drug Administration (FDA) for recanalization of arterial occlusion in patients with AIS; however, despite being cleared by the FDA, none of these devices have an FDA clinical indication due to the need for randomized comparison with medical therapy devices. Endovascular interventions are extremely time dependent, and reduced time from symptom onset to reperfusion is highly correlated with better clinical outcomes.
- CTA with CT perfusion or MRA with diffusion-weighted MRI with or without MR perfusion is recommended for certain patients (2019 AHA/ASA recommendation on head imaging).
- 2019 AHA/ASA updates on IV alteplase indications and management in acute ischemic stroke patients.
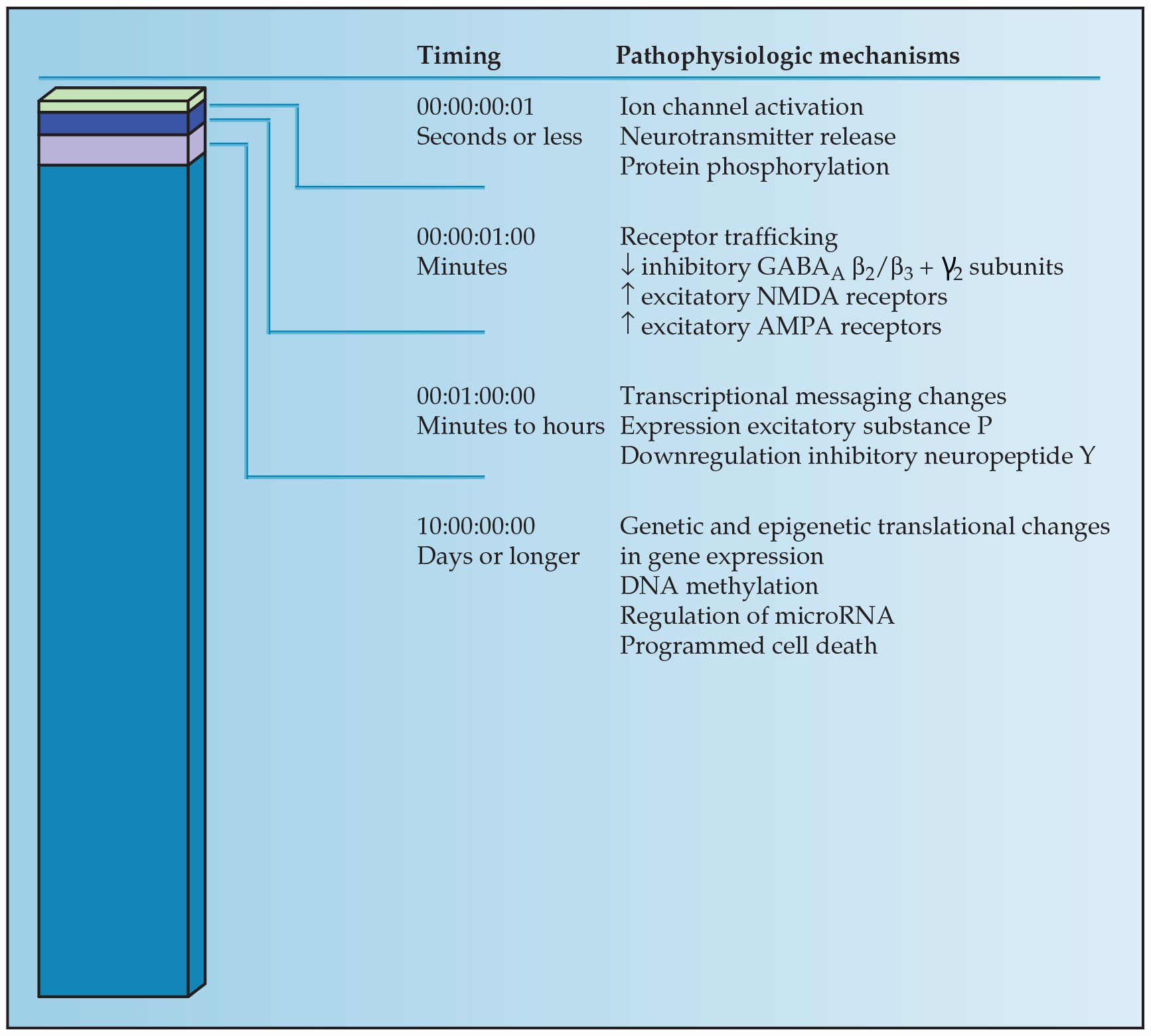
- Status epilepticus has a distinct pathophysiology that remains poorly understood; interestingly, in animal models, many of the basic underlying mechanisms appear to be common regardless of how seizures are initiated. A single seizure is transformed into a self-perpetuating and pharmacoresistant disorder through a cascade of extrinsic signaling followed by intrinsic nuclear events.
- Detailed treatment approaches for status epilepticus, delineating first-line, second-line, and third-line antiepileptic drugs.
- STESS prognostication scores primarily being used for research purposes but may have indication in clinical settings.


