Advance Directives, Do Not Resuscitate Orders, and Power of Attorney for Health Care
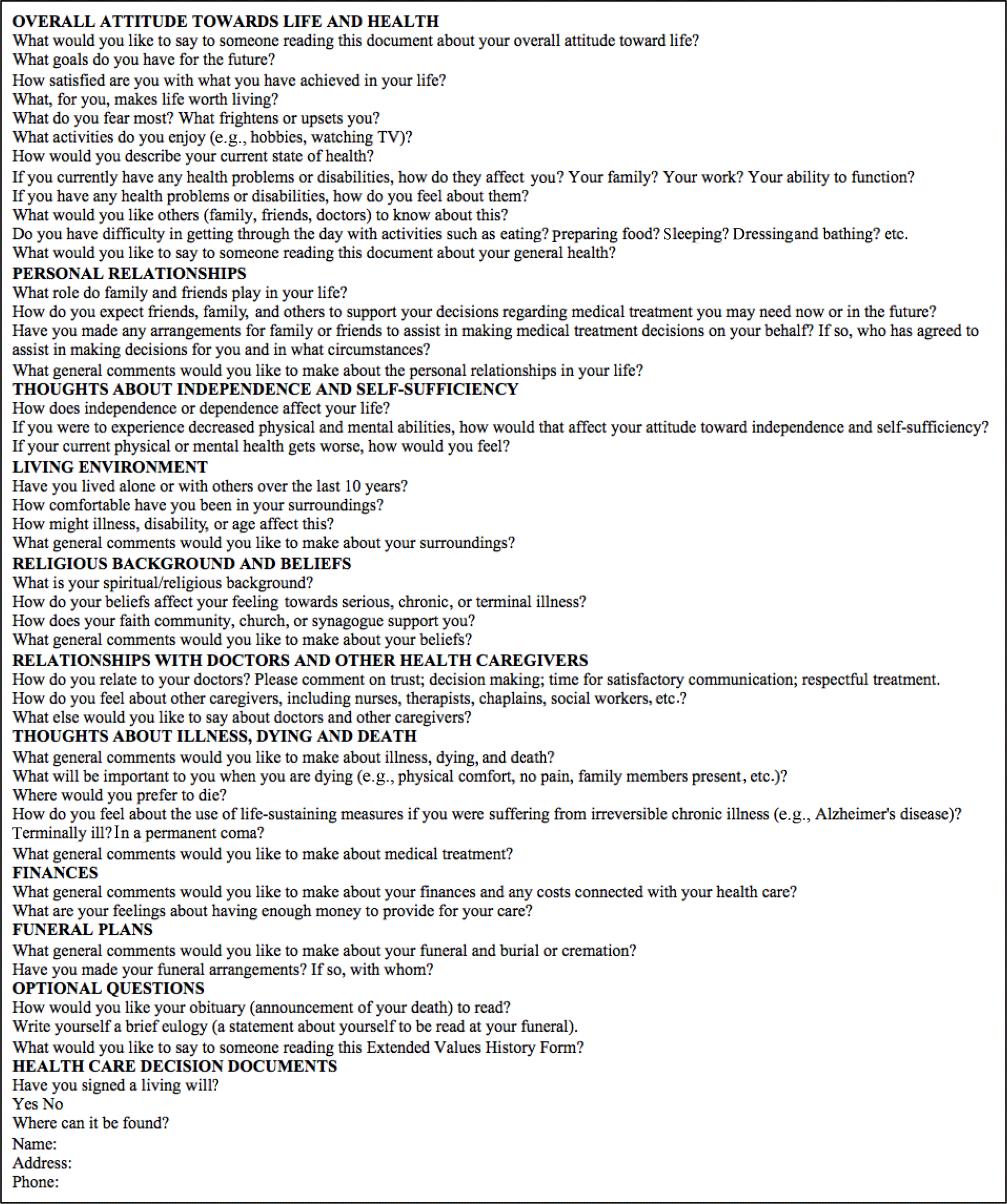
- Advance directives such as a living will, a do not resuscitate order, and a designation of a power of attorney for health care are legally binding mechanisms to preserve patient autonomy when patients have lost decision-making capacity. Although these directives are frequently used to make decisions regarding life-supporting therapy, surgeons may also need to refer to these documents or to patients’ surrogates for surgical decision making to treat patients in accordance with their autonomous wishes. There is some information to suggest that surgeons value the utility of an advance directive as it can serve as a guide to patients’ preferences in the postoperative setting when life-supporting therapy has become ineffective or patient survival is unlikely.
- The Physician Orders for Life-Sustaining Treatment (POLST) program was designed in Oregon in the 1990s to address the lack of advance directives in frail patients and those with chronic diseases. Although POLST is different from advance directives, both aim to address end-of-life care.
- When patients do not have decision-making capacity, physicians are obliged to find someone who can make decisions for the patient. If the patient has previously designated a durable POAHC agent, this agent is the first person health care providers should turn to for decision making.