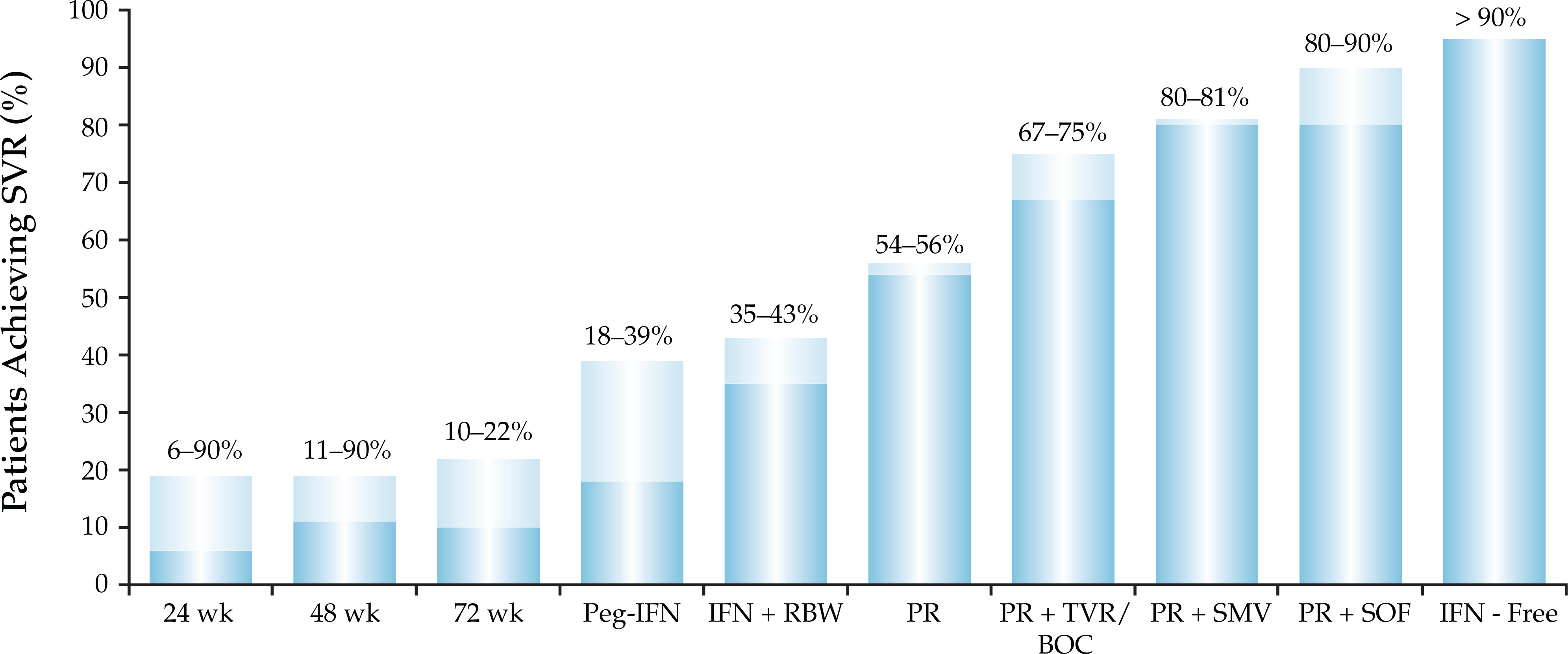
- Recent advances in treatment of chronic HCV to include interferon-free direct-acting antiviral agent regimens
- Latest treatment recommendations, including special populations
- Issues surrounding treatment-emergent resistance-associated variants
Latest Updates
Autoimmune Hepatitis/Overlap Syndromes
- Autoimmune hepatitis may have laboratory and histological features that resemble PBC or PSC, and PBC and PSC may have features of autoimmune hepatitis. These mixed clinical phenotypes constitute the overlap syndromes, and they may have a variable response to the conventional therapies used for each unmixed classical disease.
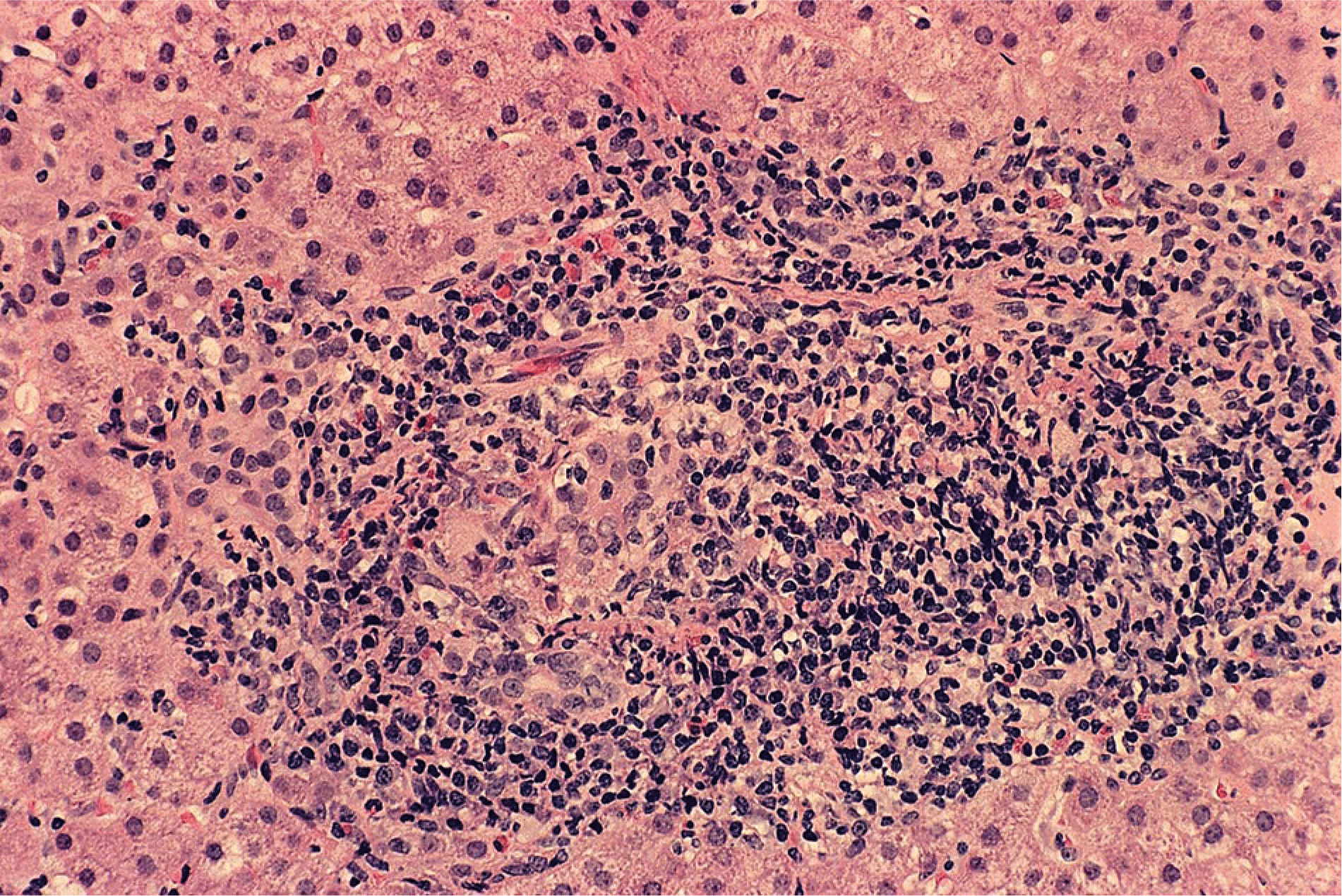
- Clinical judgment and expert interpretation of liver tissue are the principal bases for diagnosing the overlap syndromes, and incompatible manifestations of cholestasis (disproportionate serum AP and GGT elevations, destructive cholangitis or ductopenia in liver tissue) or liver inflammation (disproportionate serum AST and ALT elevations, interface hepatitis, and dense lymphoplasmacytic infiltration in liver tissue) are hallmarks of the diagnosis.
- Autoimmune hepatitis with cholestatic features that are unassociated with AMA or an abnormal cholangiography suggests the possibility of an overlap syndrome with AMA-negative PBC or small duct PSC.
- Therapy is guided by the predominant component of the overlap syndrome and consists mainly of prednisone or prednisolone, azathioprine, and low dose UDCA (13 to 15 mg/kg daily) in combination. Management strategies can be tailored to the individual patient and adjusted according to the response. High dose UDCA (28 to 30 mg/kg daily) should be avoided.
- Management of a nonresponse to the frontline regimen consists mainly of modifying the original treatment by adding corticosteroids or low dose UDCA if not present initially or considering the empirical use of mycophenolate mofetil as a substitute for azathioprine or a calcineurin inhibitor as a substitute for corticosteroids. Salvage drug therapies have had a limited clinical experience. Liver transplantation should be considered for features of liver failure.
Autoimmune Hepatitis/Overlap Syndromes
- Autoimmune hepatitis may have laboratory and histological features that resemble PBC or PSC, and PBC and PSC may have features of autoimmune hepatitis. These mixed clinical phenotypes constitute the overlap syndromes, and they may have a variable response to the conventional therapies used for each unmixed classical disease.
- Clinical judgment and expert interpretation of liver tissue are the principal bases for diagnosing the overlap syndromes, and incompatible manifestations of cholestasis (disproportionate serum AP and GGT elevations, destructive cholangitis or ductopenia in liver tissue) or liver inflammation (disproportionate serum AST and ALT elevations, interface hepatitis, and dense lymphoplasmacytic infiltration in liver tissue) are hallmarks of the diagnosis.
- Autoimmune hepatitis with cholestatic features that are unassociated with AMA or an abnormal cholangiography suggests the possibility of an overlap syndrome with AMA-negative PBC or small duct PSC.
- Therapy is guided by the predominant component of the overlap syndrome and consists mainly of prednisone or prednisolone, azathioprine, and low dose UDCA (13 to 15 mg/kg daily) in combination. Management strategies can be tailored to the individual patient and adjusted according to the response. High dose UDCA (28 to 30 mg/kg daily) should be avoided.
- Management of a nonresponse to the frontline regimen consists mainly of modifying the original treatment by adding corticosteroids or low dose UDCA if not present initially or considering the empirical use of mycophenolate mofetil as a substitute for azathioprine or a calcineurin inhibitor as a substitute for corticosteroids. Salvage drug therapies have had a limited clinical experience. Liver transplantation should be considered for features of liver failure.
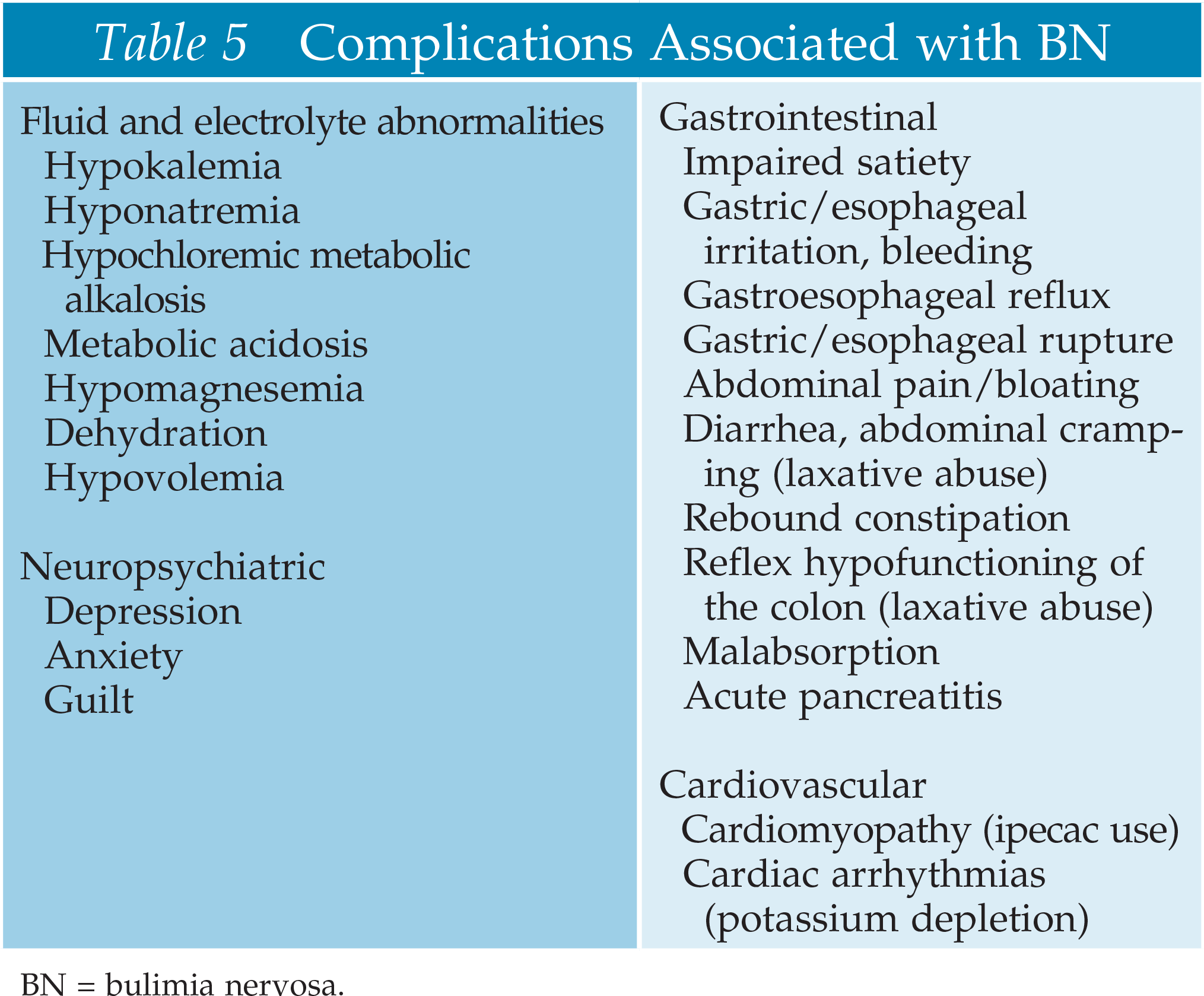
Clinical Management of Feeding and Eating Disorders
- Lisdexamfetamine for the treatment of binge eating disorder
- Novel deep brain stimulation, repetitive transcranial magnetic stimulation, and transcranial direct current stimulation
- Novel treatments for severe and enduring forms of anorexia nervosa
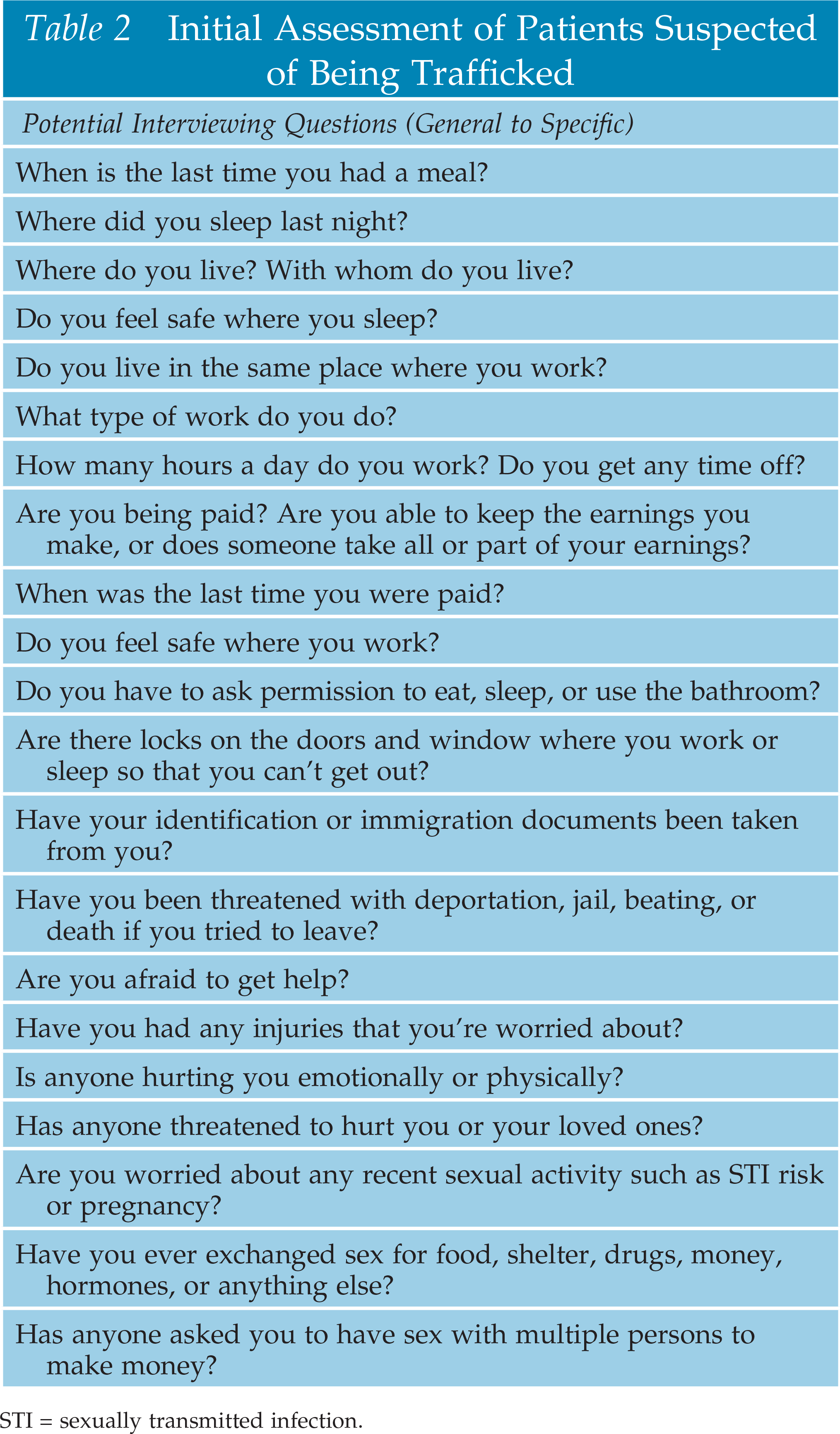
Human Trafficking 2: Approach To The Patient
- The trauma-informed approach to care has been likened to ethics of care, a philosophy that emphasizes fostering attentive, holistic, and competent patient care that is simultaneously responsive to the unique and continually changing needs, wishes, goals, priorities, risks, and vulnerabilities of the individual patient.
- ED clinicians should inform patients about their rights to privacy and the limits of confidentiality with respect to mandatory reporting laws.
- Preliminary data analysis from one clinic for trafficking victims and survivors found that 57% of trafficked persons accessed care while trafficked and 76% of them accessed care through the ED.
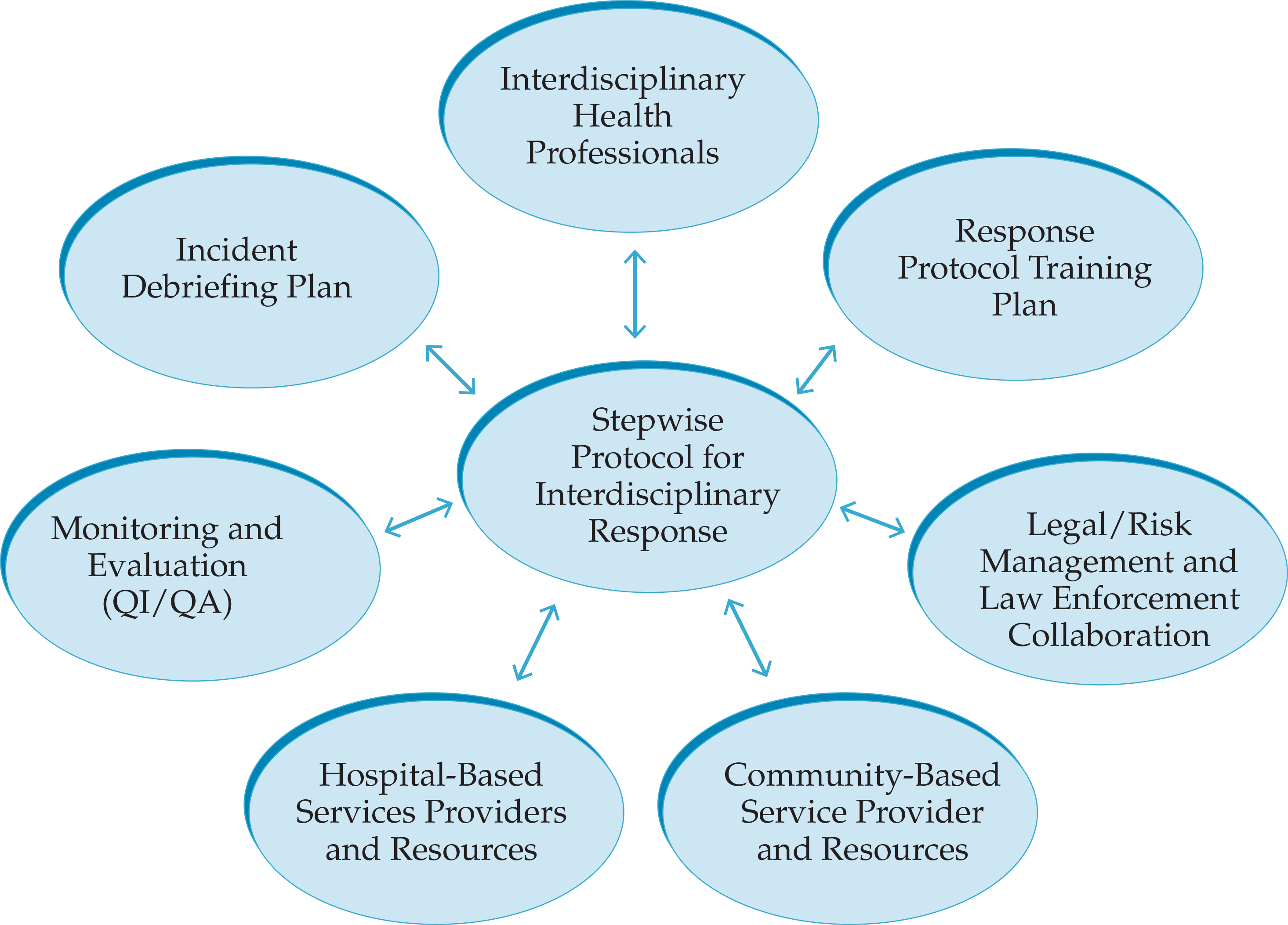
Human Trafficking 3: Intervention And Therapy
- As of May 2017, the commercial sexual exploitation or trafficking of a child under the age of 18 is considered a form of child sexual abuse under the law and would require reporting in all 50 states, the District of Columbia, and the US territories.
- If the ED physician has a concern for an active infection, testing and treatment are indicated, but in the absence of an active STI, clinicians can forego testing and counsel patients regarding presumptive treatment based on updated guidelines for antiretroviral postexposure prophylaxis following a potential sexual, injection drug use, or other nonoccupational exposure to HIV.
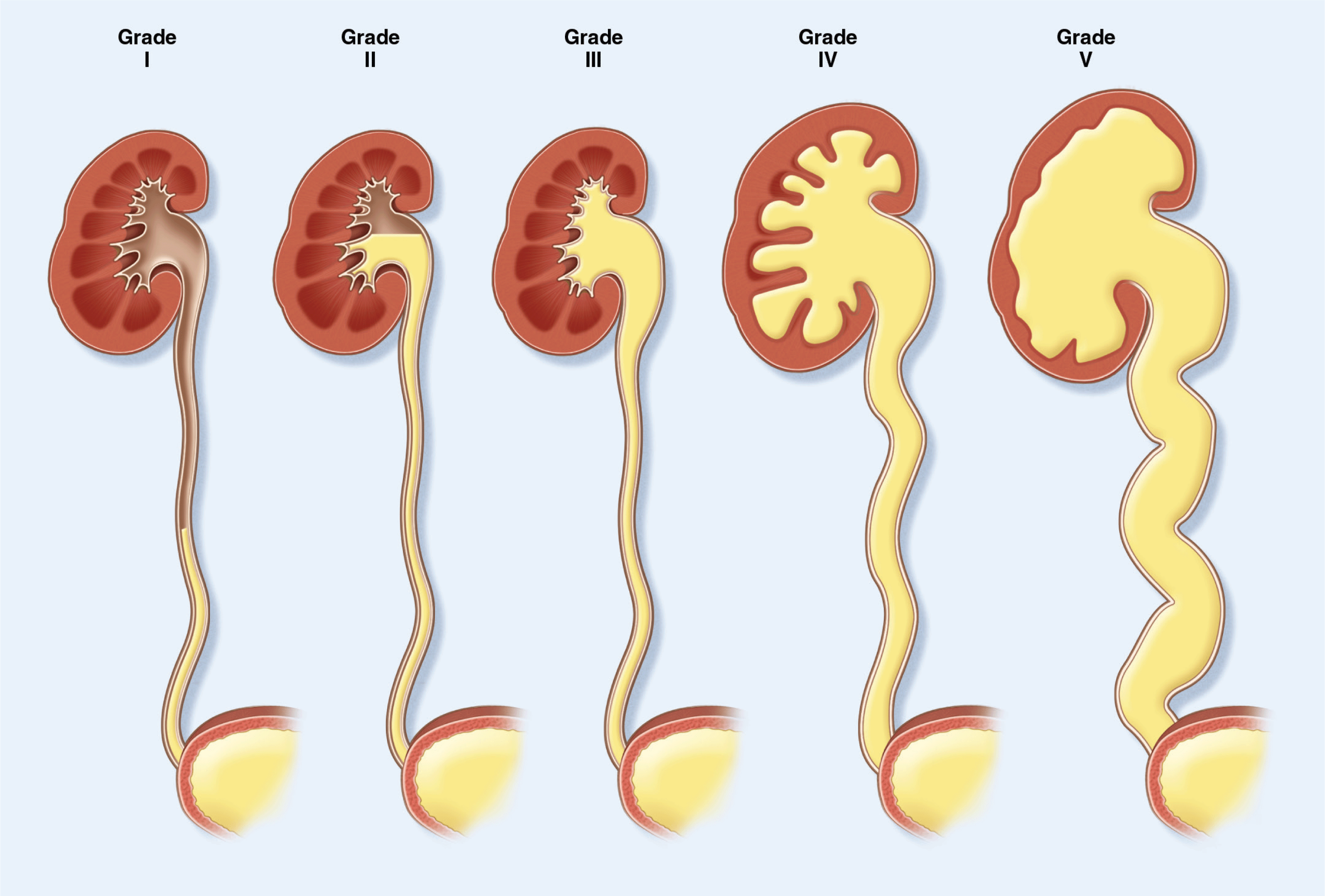
- UTI evaluation and management varies by age; rapid diagnosis and treatment prevents complications; infants may present solely with fever
- Most common uropathogen is Escherichia coli (85%). Other pathogens include gram-negative bacteria and more rarely gram-positive bacteria
- Antibiotic treatment should be based on local antibiograms plus individual patient risk factors and history
- Indications for inpatient admission include: age under 2 months, sepsis, vomiting/inability to tolerate oral antibiotics, infection with a multidrug-resistant organism, immunocompromised state, a complicated social situation, or risk of no follow up
- Risk factors for UTI in infants include age <12 months, uncircumcised males, temperature >39°C. Risk factors in adults include pregnancy, sexual activity, immunosuppression, urologic abnormalities or obstruction, long-term urinary catheter, neurogenic bladder, urinary incontinence
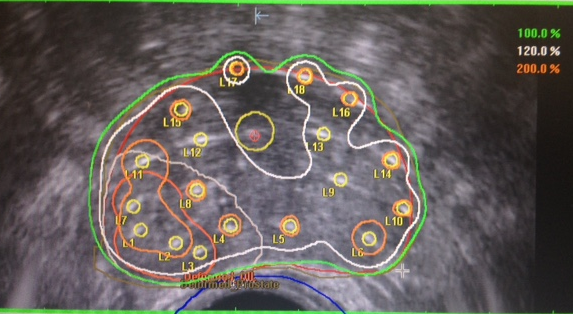
Role of Radiotherapy in Localized Prostate Cancer
- The current AUA/ASTRO consensus guidelines recommend adjuvant RT in postoperative patients with high-risk pathologic features (pT3 or positive margins).
- PSA monitoring could be an alternative; however, early administration of radiation is warranted if there is a sign of progression.
- The prognostic value of preradiation PSA is well established.
- Doses above 65 Gy to the prostate bed are recommended in the postoperative setting.
- The role of pelvic radiation is being investigated; currently, the decision is based on clinical judgment.
- Short-term ADT should be discussed with patients starting postoperative RT.


